Bone Marrow Examination (Suburban Medical Journal)
- September 15,2020
- 30 Min Read

Bone marrow is the central hemopoietic tissue found inside flat bones and the ends of long bones. It is the site of production of blood cells of all lineages viz., erythroid, myeloid and megakaryocytic.(1) Structurally It consists of hematopoietic tissue and adipose cells, intersected by vascular sinuses – all ensconced within a meshwork of trabecular bone. The hematopoietic tissue consists of a variety of cell types including, the blood cells and their precursors, adventitial/barrier cells, adipocytes, and macrophages.(2)
A bone marrow examination (morphological, flow cytometric, cytogenetic and molecular) is a critical part of the evaluation of patients with a variety of hematopoietic and non-hematopoietic diseases.(2)
Indications for Bone Marrow Examination(3,4)
- Investigation of unexplained anemia, abnormal red cell indices, cytopenias or cytoses.
- Investigation of abnormal peripheral blood smear morphology suggestive of bone marrow pathology.
- Diagnosis, staging and follow-up of malignant hematological disorders (e.g. acute and chronic leukemias, myelodysplastic syndromes, chronic myeloproliferative disorders, lymphomas, plasma cell myeloma, amyloidosis, mastocytosis).
- Investigation of suspected bone marrow metastases.
- Unexplained focal bony lesions on radiological imaging.
- Unexplained organomegaly or presence of mass lesions inaccessible for biopsy.
- Microbiological culture for investigations of pyrexia of unknown origin or specific infections, e.g. military tuberculosis, leishmaniasis, malaria, typhoid.
- Evaluation of iron stores.
- Investigation of lipid/glycogen storage disorders.
- Exclusion of hematological disease in potential allogeneic stem cell transplant donors.
- Diagnosis of metabolic bone disease and to assist in diagnosis of disseminated granulomatous disease, thrombotic thrombocytopenic purpura, primary amyloidosis.
- For bone marrow transplantation and chemotherapy of hematopoietic neoplasms or small cell tumors of childhood.
Sites of Sampling
-
Posterior superior iliac spine (PSIS)
- The posterior superior iliac spine (PSIS) is the preferred site in patients over 1 year of age.(4)
-
Anterior iliac crest (AIC)
- This site is appropriate only in adults when the posterior iliac crest is inaccessible because of obesity, infection, injury, or inability to position the patient in the lateral decubitus position.(4)
- The thick, hard cortical layer of the anterior iliac crest makes satisfactory specimens more difficult to obtain and the needle can enter the peritoneal cavity.(4)
- In addition, needle biopsy of anterior superior iliac spine has been reported to be more painful and to produce samples
-
Sternum
- Only aspiration should be attempted in the sternum; biopsies are not to be done.(4)
- Sternal aspiration should be performed only if the posterior and anterior iliac crests are inaccessible or unsuitable for the procedure.(4)
- Furthermore, sternal aspiration should be attempted only in adolescents and adults, since there is a higher incidence of serious complications in infants and children.(4)
- However, in the case of poor yield of bone marrow material from the PSIS, sternum can serve as a good source.(4)
-
Tibia
- Marrow aspiration from the antero-medial surface of the upper end of tibia is performed only in children less than 18 months of age.(4)
- The tibia is an unsatisfactory site in older individuals because of variable cellularity and the hardness of the cortical bone.(4)
Both bone marrow aspiration and biopsy are performed under local anesthesia.
Order of Performing Bone Marrow Aspiration and Trephine Biopsy
While performing both aspiration and biopsy in a patient in the same sitting, bone marrow biopsy should preferably be performed first followed by aspiration. This allows harvesting of a representative tissue in biopsy procedure without affecting representativeness of the aspirated material.(5)
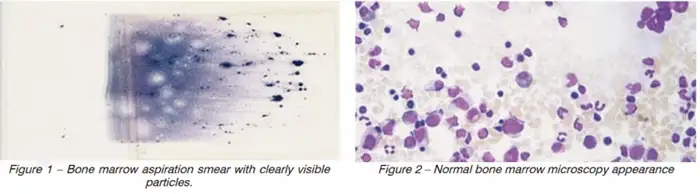
Smear preparation following Bone Marrow Aspiration/Biopsy
Preparing quality aspirate smears is an essential part of the bone marrow procedure. Smears should be immediately prepared at the bedside from the first aspirated specimen (‘‘first pull’’) to ensure adequate particles and prevent dilution with peripheral blood.(4) Only a small amount (~1 ml) of bone marrow should be drawn at one time to avoid hemodilution. This suffices for preparation of multiple smears. Larger volumes are required if additional tests such as Flow Cytometric immunophenotyping and/or Cytogenetic studies are to be performed. However, some amount of hemodilution is inevitable when large volumes of bone marrow samples are drawn.
Aspirate smears must be prepared quickly, since freshly aspirated bone marrow tends to clot fast. If smears cannot be prepared at the bedside, the aspirated material should be immediately placed into a tube containing EDTA anticoagulant (purple top) for smear preparation later in the laboratory.(4)
There are several ways to prepare smears during aspiration/biopsy. Three of the most common and easy methods of preparation (as shown below) are:
.webp)
-
Wedge technique:
- The simplest one is the traditional wedge technique used to make peripheral blood smears.(4)
- A drop of bone marrow aspirate is placed at one end of a clean microscope slide, and a second clean microscope slide is used as the ‘‘spreader slide’’.(4)
- The spreader slide is held at a 30° angle, placed in front of the drop of bone marrow aspirate, and then pulled back until it touches the drop.(4)
- The liquid is allowed to spread across the edge of the slide, which is then pushed forward using a rapid, even motion.
- The smear should end in a particle-rich feathered edge.(4)
-
Particle crush method:
- This method requires more experience to perform than the wedge preparation, but is superior for morphologic examination.(4)
- In this technique, a small drop of aspirated marrow is placed at one end of a clean microscope slide. A second clean slide is held parallel to the first slide and directly over the drop of aspirate.(4)
- With gentle pressure the second slide is pressed against the drop of aspirated marrow and pulled across the full length of the first slide to crush open and spread the marrow particles.(4)
-
Biopsy imprint (‘‘touch’’) preparations:
- These should be prepared from the bone marrow biopsy core if the aspirate specimen is devoid of particles or cannot be obtained.(4)
- In this technique, the fresh core biopsy specimen is placed on a clean microscope slide. A second clean microscope slide is pressed very gently against the biopsy core and rolled slightly from side to side. Two or three microscope slides should be prepared with several imprints on each slide. Two or three microscope slides should be prepared with several imprints on each slide. During the preparation of touch imprints, cells on the surface of the biopsy core stick to the microscope slides.(4)
Collection and preservation/transport of the Bone Marrow biopsy sample
Bone marrow biopsies should be taken with a dedicated bone marrow biopsy needle (e.g. Jamshidi needle – 8 or 11 gauge for adullts and 13 guage for the pediatric age group). The ideal biopsy sample should be minimum 1.5cm long prior to processing. The sample should then be transported in neutral buffered formalin. It is also ideal that every biopsy sample be accompanied by bone marrow aspiration smears and peripheral blood smears collected at the same time as the biopsy.
Contradictions
Bone marrow aspiration and biopsy have no absolute contraindications, but there may be relative contraindications related to the general condition of the patient or the risk of anesthesia or deep sedation: (6)
- An active infection at the proposed site of aspiration, such as the posterior iliac crest, would preclude the use of the site. However, the procedure can be performed at an alternative site if the indication for the procedure warrants it. Other sites that have been used successfully to perform aspirations include the anterior iliac crest, the manubrium of the sternum, the tibia (in infants), and, in extremely rare instances, the vertebral body.(6)
- Thrombocytopenia and other coagulopathies are not contraindications for the procedure if it is executed by a skilled clinician.(6)
- The sternum is not recommended as a site for biopsy.(6)
Complications of a Bone Marrow procedure
Bone marrow aspiration is a relatively safe procedure. However, it requires some practice and skill, acquired through performing the procedures on multiple occasions, preferably on cadavers. Complications have been documented but are rare (incidence, 0.12 to 0.30%).(6) Complications may include:
- Trauma to neighboring structures (e.g., lacerations of a branch of the gluteal artery) and soft tissues.(6)
- Infection.(6)
- Hemorrhage
- The most commonly reported complication is hemorrhage.(6)
- Risk factors for hemorrhage include thrombocytopenia, concurrent use of anticoagulants, and the presence of an underlying myeloproliferative disorder.(6)
- Retroperitoneal hematomas resulting from trephine biopsies have been reported, as have (on rare occasions) fractures of the underlying bone, especially in patients with osteoporosis/renal osteodystrophy and polycythemia vera.(4,6)
- Fatal intra abdominal hemorrhage has been reported following bone marrow aspiration and biopsy in a patient with multiple myeloma.(7)
- Unilateral lower extremity numbness and weakness following the bone marrow examination, presumably from infiltration of the sacral nerve plexus.(4)
- Breakage of the bone marrow needle or separation of the handle during insertion into the bone is a very rare complication of marrow procurement.(4)
References
- Bain BJ, Clark DM, Wilkins B. Bone marrow pathology. 4th ed. Chichester, UK ; Hoboken, NJ: Wiley-Blackwell; 2010. 630 p.
- Travlos GS. Normal Structure, Function, and Histology of the Bone Marrow. Toxicol Pathol. 2006 Aug;34(5):548–65.
- Lee S-H, Erber WN, Porwit A, Tomonaga M, Peterson LC, International Councilfor Standardization In Hematology. ICSH guidelines for the standardization of bone marrow specimens and reports. Int J Lab Hematol. 2008 Oct;30(5):349–64.
- Riley RS, Hogan TF, Pavot DR, Forysthe R, Massey D, Smith E, et al. A pathologist’s perspective on bone marrow aspiration and biopsy: I. performing a bone marrow examination. J Clin Lab Anal. 2004;18(2):70–90.
- Kaushansky K, editor. Williams hematology. Ninth edition. New York: McGraw-Hill; 2016. 2 p.
- Malempati S, Joshi S, Lai S, Braner DAV, Tegtmeyer K. Bone Marrow Aspiration and Biopsy. N Engl J Med. 2009 Oct 8;361(15):e28.
- Gupta S, Meyers ML, Trambert J, Billett HH. Massive intra-abdominal bleeding complicating bone marrow aspiration and biopsy in multiple myeloma. Postgrad Med J. 1992 Sep 1;68(803):770–770.
Want to book a test? Fill up the details & get a callback
Most Viewed
Premarital Health Screening
- 20 Min Read
Typhoid - Signs and Symptoms
- 3 Min Read
Home Isolation Guidelines - Covid-19 Care
- 5 Min Read
HLA B27 Detection: Flow Cytometry & PCR
- 1 Min Read














